|
Before COVID-19, there was a growing concern that many individuals who suffer from osteoporosis had experienced adverse issues with prescribed medications, and were therefore avoiding seeking treatment. Now, with the disruption to the health system by the pandemic, the situation has only gotten more complicated, and potentially dangerous, for these patients.
For that reason we thought it would be good to update our article from last year to include new clinical guidance on managing osteoporosis patients that takes the so-called "new normal" into account.
Osteoporosis is a disease of the bone that makes a person’s bones weak and more likely to break. Approximately 10 million Americans have osteoporosis and another 44 million over age 50 have low bone density, placing them at increased risk of fracture, according to the National Osteoporosis Foundation NOF). Further, one in two women and up to one in four men will break a bone in their lifetime due to osteoporosis. Diet, exercise and a healthy lifestyle are keys to preventing and managing the disease.
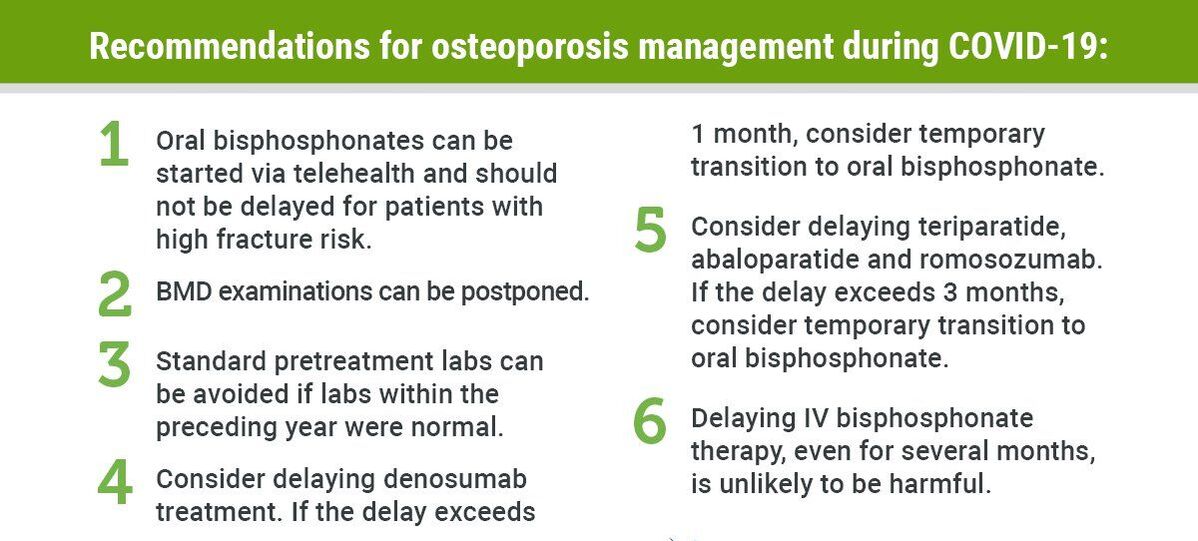
In May, a coalition of leading bone health organizations released new guidance for clinicians treating patients with osteoporosis in the era of COVID-19. The joint guidance -- from American Society for Bone and Mineral Research (ASBMR), American Association of Clinical Endocrinologists (AACE), Endocrine Society, European Calcified Tissue Society (ECTS) and NOF -- outlines important treatment adjustments for osteoporosis therapies and alternative methods for assessing fracture risk in the absence of a bone density (DXA) scan.
“It is important people with osteoporosis stay on top of their medical care and stay in the medical routine," said Suzanne M. Jan De Beur, MD, associate professor of medicine at the Johns Hopkins University School of Medicine and incoming president of ASBMR in a recent article on about the guidelines. "Clinicians must ensure patients take their medications and that they have access to the medications. If clinicians must modify osteoporosis therapy because a patient cannot come in for injections, follow the guidance or put them on a bridge therapy to keep them from losing bone.”
A crisis in treatment before COVID
But the COVID crisis is just the latest chapter in the ongoing challenge of helping osteoporosis patients get the treatment they need. Orinda, California, internist Elliott Schwartz, MD called it “a current treatment gap or crisis in treatment or lack of treatment” for individuals who have the disease. As medical director of the Northern California Institute for Bone Health, Dr. Schwartz also works with the UCSF Skeletal Health Service.
According to Dr. Schwartz, the treatment crisis came about due to the aging of our population and the fact that many individuals who suffer from osteoporosis have had adverse issues with prescribed medications, and have stopped seeking treatment. The decrease in the rate of treatment over the last several years has spawned a large increase in the number of hip fractures in the aging population. “Practitioners need to help their patients understand what the issues are,” he says. “People don’t trust the treatment they have received, so have become afraid of these medications and their negative side effects. Yet, most of the time, in my opinion, things can be done to ameliorate the situation and reduce the potential for these adverse reactions. For example, I recommend reducing the dose by half (e.g., from 70 mg to 35 mg a week) of alendronate, a class of medications called bisphosphonates that is used in osteoporosis treatment. “In addition, we have new medicines, called anabolic medicines, or bone builders, that can be used before taking a bisphesphemate drug for a better result or outcome. These include teriparatide (Forteo) and abaloparatide (Tymlos™). Neither is associated with the rate of side effects that many osteoporosis patients have experienced.” Dr. Schwartz points to studies that show that 25% of patients who have had a fracture are likely to have another fracture in the next year, and 50% will experience a new fracture in five years. “These statistics offer a good reason to get into treatment and not to become afraid and do nothing,” he says. Vitamin D and exercise
He also stresses the importance of getting an adequate amount of Vitamin D each day and the value of physical exercise. "Patients should be referred to physical therapy for strengthening exercises, he notes. “In a new area of research in sarcopenia, the degenerative loss of skeletal muscle mass, we have learned that people lose about 40% of their muscle mass from age 40 to age 70 or 80. To prevent this loss or reduce its progression, people need to exercise in their old age. While exercise does not build your bones, it helps you keep your muscle strength intact, so you can maintain agility and coordination. This means you will fall less often, thereby reducing fractures.”
In addition to the Northern California Institute for Bone Health, more information about osteoporosis and its treatment is available at the National Osteoporosis Foundation and the Mayo Clinic. (If you find other great sources of information, please share them with us.) Comments are closed.
|
AuthorsWe're the staff and volunteers at Jackson Orthopedic Foundation, committed to improving the lives of patients with musculoskeletal conditions through education, research and service. Archives
July 2024
Categories
All
|
|
|
Jackson Orthopedic Foundation
400 30th Street, Suite 102 Oakland, California 94609 510.238.4851 Our live courses are taught in Lafayette, California
|


 RSS Feed
RSS Feed